 Every day, your feet take between 8,000 and 10,000 steps. No wonder then, that any structural problems, such as flat feet or improper walking patterns, can cause pain and soreness. Toss in the large amount of running and aerobic exercise that people take part in, and it’s clear that healthy feet are essential. Foot structure and the way you walk can also affect the health of your back, knees and legs.
Every day, your feet take between 8,000 and 10,000 steps. No wonder then, that any structural problems, such as flat feet or improper walking patterns, can cause pain and soreness. Toss in the large amount of running and aerobic exercise that people take part in, and it’s clear that healthy feet are essential. Foot structure and the way you walk can also affect the health of your back, knees and legs.
Your chiropractor is trained to identify problems with your feet and associated body parts that are contributing to your foot discomfort. Your chiropractor will carry out a thorough examination to help identify the structures involved. He or she may use adjustments, physiotherapeutic modalities, such as ultrasound, or recommend orthotics and exercises to help to prevent future injuries.
PES PLANUS
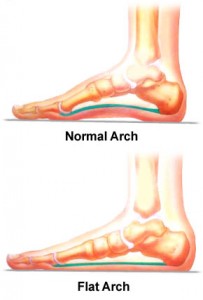 Pes planus, often called flat feet, is very common. Some research estimates that one quarter of the population has flat feet. In fact, we’re all born with flat feet and only as we age, somewhere between age 3 and 10, do our feet usually develop an arch.
Pes planus, often called flat feet, is very common. Some research estimates that one quarter of the population has flat feet. In fact, we’re all born with flat feet and only as we age, somewhere between age 3 and 10, do our feet usually develop an arch.
Some people never grow arches, however, and others experience fallen arches, which occurs when the arch develops but later collapses. It’s not difficult to know if you have either of these problems. While seated, with your feet flat on the ground, bend down and look at the inside of either foot. If you don’t have the condition, you should see a raised area in the middle. If the whole foot is relatively flat on ground, however, and there’s little or no noticeable rise where the arch should be, you probably have flat feet.
While recognizing flat feet might be easy, predicting its long-term effects is more difficult. Over time, flat feet can cause pain, but it’s possible for people to have the condition and never feel any discomfort. For people who do develop pain, it usually occurs in the feet and knees, and possibly in the hips and lower back. The discomfort or irritation in any one of these areas can vary immensely. The pain in the foot, for example, can feel sharp, dull, bruised, achy or tight.
Besides genetic causes, which prevent people from ever developing arches, there are a number of factors that can cause flat feet or predispose people to the condition. Structural abnormalities in the feet such as over-pronation, which involves the foot rolling too far inward, are one cause of the condition. Activity level also contributes. People who are regularly involved in athletic activities or work at a job that requires them to remain standing for extended periods are more likely to have flat feet and experience pain from the condition, as it makes them more susceptible to soreness in the feet, knees, hips or low back. Those who aren’t active, on the other hand, may have weak muscles that are less capable of supporting the arches, which therefore allows the feet to weaken.
Age and weight also play a role in the condition’s development. Middle-aged people who have been working on their feet for years often experience flat feet, as do overweight people who are placing added stress on their feet and legs. Both prolonged standing and excess weight can put stress on the body that forces the legs and feet to do more work than they’re capable of.
If you have flat feet, you should see your healthcare practitioner as soon as possible regardless of how much pain the condition’s causing. Your healthcare practitioner can determine a plan of management that can ease pain or prevent symptoms from developing.
PLANTAR FASCIITIS
If you long for days when getting out of bed wasn’t so tough on your feet, you may be suffering from plantar fasciitis.
you may be suffering from plantar fasciitis.
Patients with plantar fasciitis often complain of such foot pain after standing up in the morning or after a long period of sitting. The pain originates just in front of the heel bone, but can spread over the entire bottom of the foot. Over time, inflammation associated with the condition can lead to the development of scar tissue, calcium deposits and eventually a heel spur, which is a bony growth that can cause a sharp stabbing pain every time people with the condition walk.
Plantar fasciitis often develops in people who have other foot conditions, especially pes planus (flat feet) and over-pronation. Flat feet are feet that have little or no arch, while over-pronation occurs when the foot rolls too far inward when people walk. Both of these conditions can cause excess stress on the plantar fascia and lead to a mild form of plantar fasciitis.
A number of factors can exacerbate plantar fasciitis in those with preexisting conditions, as well as cause plantar fasciitis by themselves. People who are constantly on their feet, such as nurses, teachers and waiters, are more susceptible, as are athletes who participate in foot-stressing activities such as aerobics, volleyball, running, basketball and tennis.
Many other factors also put excess stress on the feet and cause or contribute to plantar fasciitis. Sudden strenuous activity after a period of long-term inactivity, abnormal walking patterns, improper footwear, walking on hard or uneven surfaces, weak foot muscles, muscle imbalances and obesity are among the chief culprits.
The thing that unites these factors is that they overwork the plantar fascia, which is a band of connective tissue that surrounds the muscles on the bottom of the foot like plastic wrap. The plantar fascia runs from the heel to the forefoot, connecting the heel bone to the ball of the foot, supporting the arch, protecting the foot and absorbing shock. Any abnormal stress related to preexisting foot conditions or excess activity can strain the plantar fascia and lead to irritation, inflammation and severe pain.
Depending on which factors caused the condition, healthcare practitioners tend to care for plantar fasciitis with different techniques. And since everyone’s case is unique, there is no specific timeline outlining when the foot will heal. Once your healthcare practitioner determines the underlying cause or causes, however, he or she will develop a management program that will quickly decrease inflammation, which is the first step to decreasing pain.
METATARSALGIA
Metatarsalgia is sometimes called ball-of-foot pain, which is appropriate  considering that people with this condition often feel pain around the ball of their feet. But even though people feel pain there, the actual problem begins higher up, in the metatarsal bones that compose large portions of the feet.
considering that people with this condition often feel pain around the ball of their feet. But even though people feel pain there, the actual problem begins higher up, in the metatarsal bones that compose large portions of the feet.
If you look down at your bare feet and point your toes up, you can probably see some of these bones. They’re the five bones in each forefoot that extend from about half way up the foot to the toes.
While many patients with metatarsalgia feel pain where their metatarsal bones join their toe bones, some also feel pain along the entire length of the metatarsals and possibly between them. And this pain can vary depending on the cause of the condition. If your forefoot feels stiff or sore when you move it, joint dysfunction is probably causing your metatarsalgia. If you feel burning or stinging, nerve damage is probably responsible.
A number of internal and external factors can cause these problems. Internal factors can be structural, functional or both. Structural problems refer to abnormalities in the metatarsals themselves. If, for example, someone’s metatarsals grow too long, it could change the mechanics of his or her feet and lead to abnormal movements that strain the forefoot and possibly cause joint dysfunction. Functional problems refer to abnormalities in other foot structures that then affect the metatarsals and cause metatarsalgia. If, for example, someone has flat feet, the lack of arches could affect how he or she walked, putting excess strain on the metatarsals.
External factors include excess body weight, tight or high-heeled shoes and repetitive foot activity. Excess weight can overload the metatarsals and affect the way people walk, which can cause joint pain and nerve irritation. High-heeled shoes stress the metatarsals, because the raised heel channels the majority of pressure from walking onto the front of the foot. Repetitive foot activities, like running, directly stress the metatarsals by exposing them to constant trauma.
Regardless of the cause, your healthcare practitioner can effectively care for metatarsalgia. After determining what factors are underlying your condition, he or she can offer a variety of non-invasive therapies as well as advice on how you can avoid future pain.




FOLLOW US!